Manual Lymphatic Drainage Massage
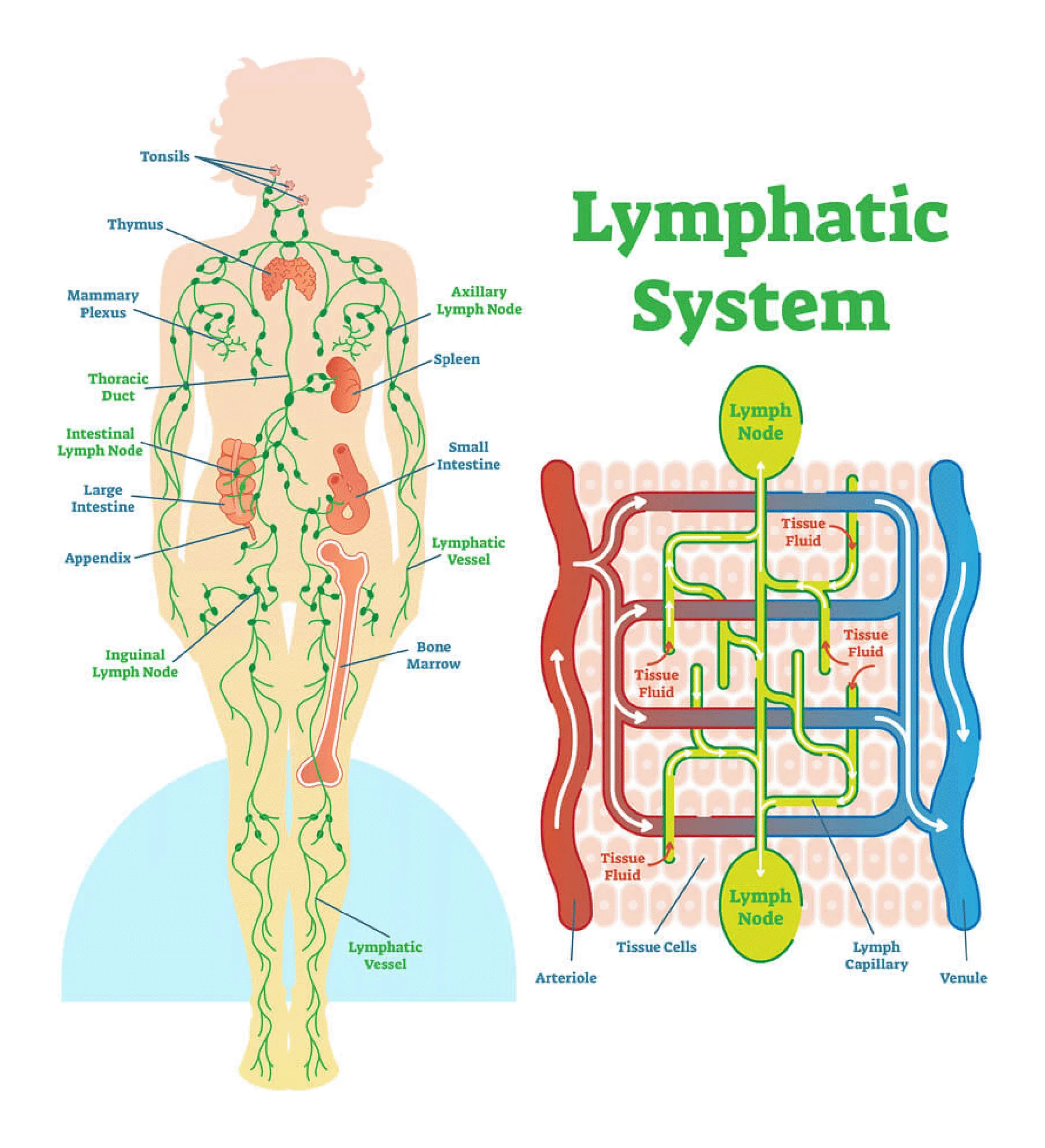
A gentle form of bodywork that stimulates the lymphatic system to reduce edema/excess inflammation, remove toxins and waste, and encourage a healthy immune system. This type of treatment is appropriate for most people (see contraindications). Very beneficial for patients: post-cancer, with lipidema/lymphedema, post-surgical, with autoimmune conditions, long COVID, with systemic inflammatory conditions such as Lyme, PCOS, endometriosis, and many more.